 The COVID-19 pandemic has brought intense scrutiny of our hospital systems, especially what happens when adults over age 80 or living with complex acute illness are facing hospitalization. The decisions a relatively healthy person might make without blinking require careful consideration when it is an older adult living with life-limiting illnesses like congestive heart failure or chronic obstructive pulmonary disease.
The COVID-19 pandemic has brought intense scrutiny of our hospital systems, especially what happens when adults over age 80 or living with complex acute illness are facing hospitalization. The decisions a relatively healthy person might make without blinking require careful consideration when it is an older adult living with life-limiting illnesses like congestive heart failure or chronic obstructive pulmonary disease.
Here are four things to consider when facing hospitalization due to COVID-19:
- Be upfront with medical providers right from the start of the admission process. They will look at what we call their ADLs, or activities of daily living: Do they need to use a walker or wheelchair? Are they able to get around independently, prepare their own meals, bathe and dress themselves? Someone in their 80s or 90s who functions as if they are in their 60s or 70s will have a different conversation about treatment options. If the patient has end-stage dementia or other progressive illness, is bed bound, and does not have that degree of functionality, then a serious conversation is needed about whether intubation or mechanical ventilation is a wise decision from a quality-of-life perspective. One of the questions should be is, if you intubate them will they ever be able to get off the vent? Is that something that grandma or dad would have wanted in the first place?
- The straight talk you have from the beginning is part of what helps providers determine what they call “goals of care.” This is defining the focus of the patient’s care. The first step is understanding the patient’s medical issues and conversations with the patient, family and other medical providers. The second step is what procedures and treatments you would or would not want done, especially factoring in the patient’s condition prior to hospitalization. The goals of care for let’s say a urinary tract infection is different depending on each patient. For a 40-year-old man in average health, you have a choice of a half dozen antibiotics. With an octogenarian with several complex medical conditions who has had prior infections and hospitalizations, you are limited to perhaps one IV antibiotic, and even that has a lot of side effects including things like seizures and renal failure. You have the same diagnosis resulting in two very different goals of care.
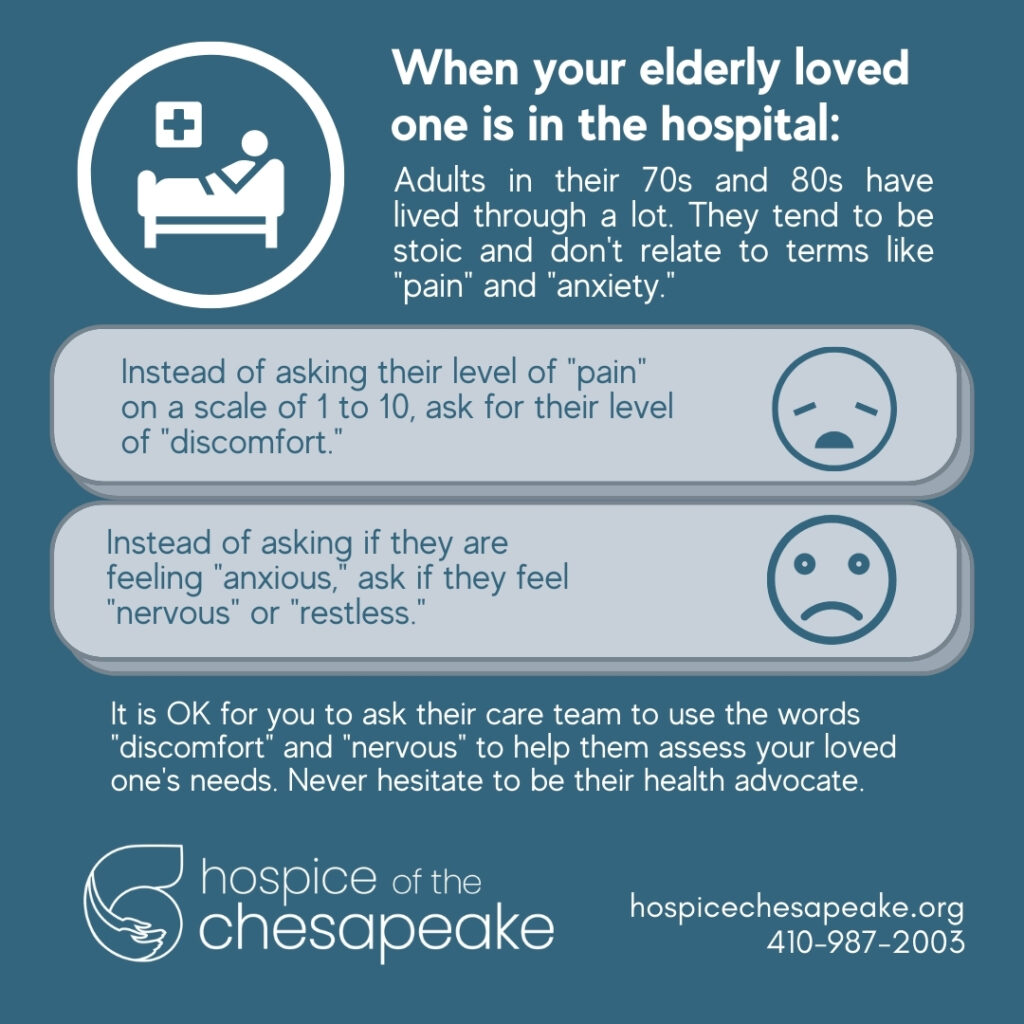
- It’s OK to ask the hospital care team to use language they can understand or relate to. That applies to any age, but folks who are 80 and older tend to be rather stoic to get to that age. They tend to minimize the everyday aches and pains, shortness of breath, just to keep going. That is a healthy thing for them to do in the everyday, but in a crisis situation, the medical team needs to know how to help them. If you ask them if they are in pain, almost always, they will tell you “No.” If you ask them if they are in any discomfort, they will admit to that. The same goes with the word “anxiety” – it is not a word they use. Instead ask if they are feeling nervous or restless.
- Visitor restrictions may be the hardest part of pandemic hospitalization. Nothing can replace being surrounded by friends and family to bring comfort, but a close second is taking advantage of today’s technology for virtual real time visits. Care teams have smart devices that allow patients to talk with family and friends via FaceTime, Zoom or Google Duo. If you are able to see them and how they are doing, it is an affirmation of whatever written or verbal reports you’re getting from the care team. Also, reach out to get the perspective from the psycho-social members of the care team – the social worker and the chaplain. It will help you gain a more 360-degree view of not only the physical, but emotional and spiritual health of your loved one.
Perhaps the greatest takeaway from this time in our history is how important it is to make critical healthcare decisions now and to document and share them with your family. It is an act of love to let them know in advance what you would decide if facing hospitalization.


